Amy Stephens
MS, RDN, CSSD, CEDS
Licensed dietitian
specializing in sports nutrition
and eating disorders
MS, RDN, CSSD, CEDS
Licensed dietitian
specializing in sports nutrition
and eating disorders
We all know far too well that gastrointestinal issues can derail a training run or race physically and mentally. Cramping, bloating, and diarrhea can quickly worsen dehydration and become very painful or even debilitating. In this post, I outline some easy strategies to help you feel better and improve performance when facing GI issues. By following these nutrition strategies, one can improve symptoms and performance as a whole.
GI issues can happen before, during, or after a run and can rapidly cause dehydration and electrolyte imbalance. If GI issues are not addressed, they can lead to underfueling, cramping, and poor performance. Underfueling will eventually lead to hitting the wall, or even dropping out of a race altogether.

Why do GI issues happen with some athletes?
There are a few reasons for GI issues in runners.
Nutrition strategies to prevent GI issues:
It’s important for athletes to ensure they’re hydrated before heading out for a run. When exercising, the blood is shunted to working muscles and away from the gut causing a lower blood volume. Ultimately, any food or sports beverage you consume during a workout may cause GI distress.
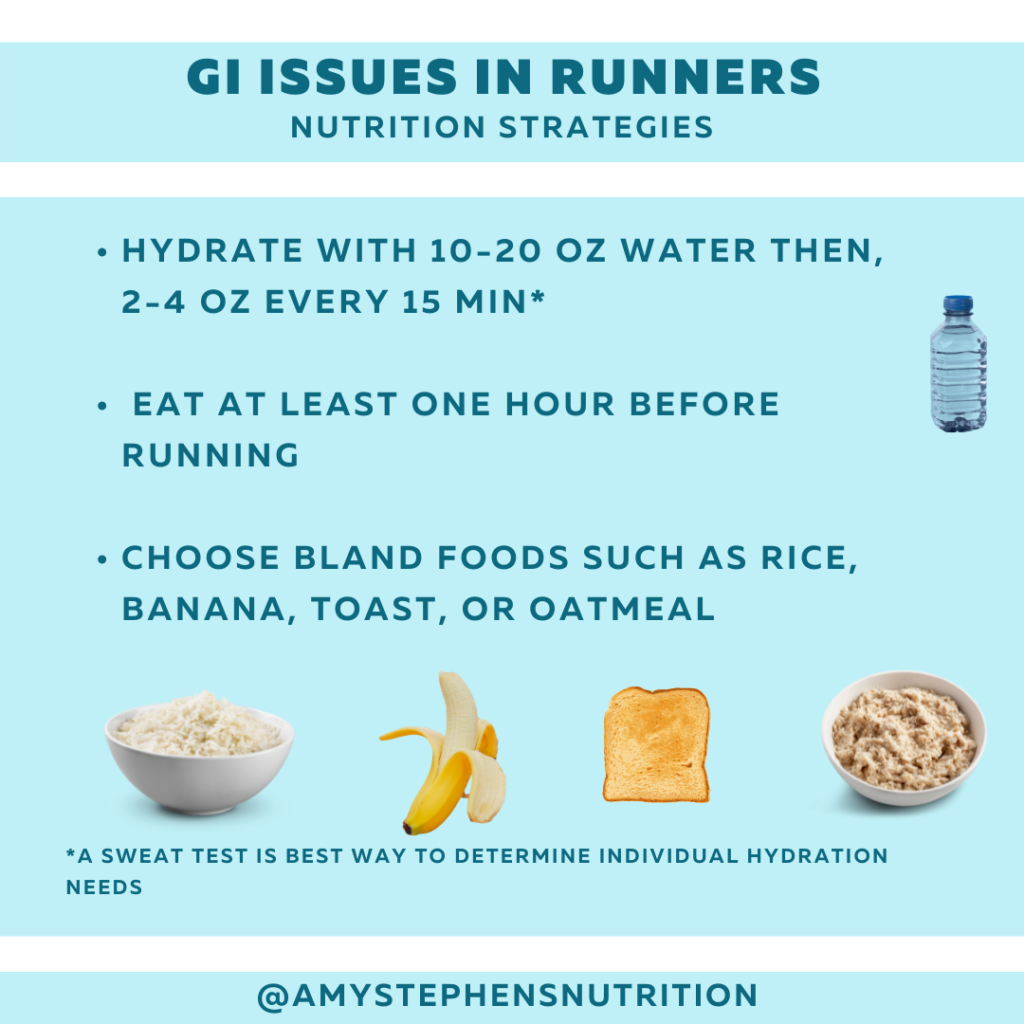
1. Time meals so you finish eating at least one hour before running. Work with a sports dietitian to time your food so it’s digested by the time you start exercising.
2. Hydrate by drinking 10-20 oz of water one hour before a run and 2-4 oz every 15 min for runs lasting one hour or longer. You might need to do a sweat test to see how much water your body loses. Take note that you lose more water when exercising in hot, humid, dry, and high altitude.
3. Experiment with different foods to find what works best for your body.
4. Foods – Include bland foods such as, rice, bananas, oatmeal, dry toast, or potatoes before your run. Another dietary strategy is called Low Fodmap which has been shown to help with GI symptoms. I’ll write more about this and how to follow in a separate post.
Quick tips:
Try these gu’s, gels, and chews during your run because they are made with fewer processed ingredients. Instead of maltodextrin, they use monosaccharides like glucose and fructose which are easier for the body to digest. They are best tolerated with a gulp of water.
Try these Gels, Gu’s or chews
Gels/Gu’s
Honey stinger – website
Untapped energy gels – website
Huma energy gels – website
Energy chews are great because you can ingest them at a slower rate. This allows your gut to work more slowly and not cause GI issues. For best results, you may take a few at a time.
Liquid sports drinks such as Skratch or Maurten can be helpful because they are hydrating and can be taken in a small amount at a time. When using, be careful not to overwhelm the gut by ingesting too much too fast.
You can also ask your doctor about the over the counter medication called imodium.
References
Gibson PR, et al. Other dietary confounders: FODMAPS. Dig Dis. 2015;33(2):269–276.
Lis DM. Exit Gluten-Free and Enter Low FODMAPs: A Novel Dietary Strategy to Reduce Gastrointestinal Symptoms in Athletes. Sports Med. 2019 Feb;49(Suppl 1):87-97.
O’Keeffe M, Lomer MC. Who should deliver the low FODMAP diet and what educational methods are optimal: a review. J Gastroenterol Hepatol. 2017;32(Suppl 1):23–26.
Staudacher HM, et al. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. 2011 Oct;24(5):487-95.
Licensed Dietitian Specializing in sports nutrition and eating disorders
© Amy Stephens Nutrition
Website by Second Language